In a previous article on urinary incontinence, I shared how it is the shameful secret that many women keep hidden. Despite the fact that a majority of women will experience urinary incontinence in their lifetime, the progress in understanding the underlying causes has been slow. As a result, diagnosis and treatment remain fundamentally the same – and woefully inadequate for millions of women.
In a previous article on urinary incontinence, I shared how it is the shameful secret that many women keep hidden. Despite the fact that a majority of women will experience urinary incontinence in their lifetime, the progress in understanding the underlying causes has been slow. As a result, diagnosis and treatment remain fundamentally the same – and woefully inadequate for millions of women.
Unfortunately, this is a pattern I see throughout so many health issues impacting women. We are still too often regarded as “too complicated” for research. We are still told these are just “women’s issues” and they are part of life. We are told not to discuss sexual function, menstrual and pelvic pain, menopausal issues … or anything that makes people uncomfortable – including the very healthcare practitioners responsible for providing women’s health care.
Part of the reason these issues make people uncomfortable is our societal view of women, their bodies, and their right to have answers to their questions and concerns. Women’s sexual health and functioning are often not given the attention and respect they deserve – in research, in clinical care, in societal values. If we had put even a fraction of all of the money that has gone into researching and treating male erectile dysfunction into women’s health issues, I would be writing a different article.
When it comes to pelvic support and urinary incontinence, the standard diagnostic evaluations are woefully inadequate. Urodynamics and pelvic exams are both intrusive and have a low level of accuracy. Urodynamic evaluation, an invasive procedure still considered the “gold standard” for evaluating urinary incontinence, is unable to provide a reliable diagnosis half the time. [1] The clinical parameters for the standard measurement of pelvic organ support is based on expert opinion, and is limited by ability to examine the pelvis in supine vs standing positions – important because gravity influences the findings. Neither evaluates the underlying anatomy, looking at the surface view rather than the pelvic support tissues themselves.
We need to find better ways to understand the underlying pathologies and how they contribute to pelvic floor issues that contribute to urinary incontinence, including prolapse. Not surprisingly, there are noninvasive technologies that already exist, but we aren’t using them.
 Imaging techniques, including CT, MRI and ultrasound have all been shown to provide helpful information related to these hidden tissues and structures. [2] Each is noninvasive, and shown to be superior to the current standard evaluations, but they are not widely used and have limited research linking the findings to effective treatments. Cost is one factor – CT and MRI are more expensive and must be done within a facility that has this equipment. They are also limited by the fact that they are static imaging technologies, unable to capture the dynamic changes that happen with the Valsalva maneuver (bearing down) or gravity.
Imaging techniques, including CT, MRI and ultrasound have all been shown to provide helpful information related to these hidden tissues and structures. [2] Each is noninvasive, and shown to be superior to the current standard evaluations, but they are not widely used and have limited research linking the findings to effective treatments. Cost is one factor – CT and MRI are more expensive and must be done within a facility that has this equipment. They are also limited by the fact that they are static imaging technologies, unable to capture the dynamic changes that happen with the Valsalva maneuver (bearing down) or gravity.
Ultrasound is a technology that is common in most ObGyn offices, and many urology offices – the two specialties that address pelvic floor and incontinence issues. 3D ultrasound has been shown to be highly accurate in assessing the pelvic floor structures. It is relatively inexpensive, dynamic, quantifiable and reproducible. [See: ITN feature -Digital Imaging for Pelvic Floor Disorders 9/15/2022]
If integrating 3D ultrasound into evaluating pelvic floor support and incontinence seems like a no-brainer, you’re right. So why aren’t we making better progress?
The same reason we are still so much in the dark ages with women’s health.
The impetus to advance the research and implementation of newer and better approaches fails when it comes to the halls of power. Research is still very much dominated by men from top to bottom – determining the policies, funding research grants, conducting clinical trials, research participants, publishing results. Even moving past this hurdle, there is the issue of healthcare spending coverage and priorities.
But we can change this. In order the shift the conversation, we need to shift the power.
It starts with being willing to challenge the status quo. Asking the right questions. Dedicating the resources needed to explore and research. Moving beyond our individual silos of expertise to initiate a more collaborative approach to finding answers.
1) Palaiologos, K., Annappa, M., & Grigoriadis, G. (2019). Correlation Between Urodynamic and Clinical Diagnoses in Classifying the Type of Urinary Incontinence in Women. Cureus, 11(10). https://doi.org/10.7759/cureus.6016
2) Shek, K. L., & Dietz, H. P. (2016). Assessment of pelvic organ prolapse: A review. Ultrasound in Obstetrics & Gynecology, 48(6), 681-692. https://doi.org/10.1002/uog.15881
Why I wear Pull-Ups… By: Jesi Stracham
When Depends became too baggy after my weight loss causing leaks and the pads would slide to the side, I switched to GoodNites brand children’s diapers. Immediately, my confidence was boosted with the cute designs and panty like fit. Even though I have my bladder well managed, I still wear them daily. With my active lifestyle I like the piece of mind that if I have an accident my wheelchair cushion and clothes will still be dry. I simply rip the diaper off, clean my downstairs “area” with a baby wipe, put a new diaper on and wheel on my way.
Often times SCI survivors suggest Botox Injections and pharmaceuticals to help with my incontinence. I used both up until April 2017 when they quit working. I searched high and low for natural alternatives after realizing how well my body felt after getting off of the pharmaceuticals. The uncomfortable constipation and dry mouth ceased within days!
Early summer 2018 I had a bladder study done. The nurse who perform the study shamed me for refusing to take the prescribed medicines. She put me in tears saying due to the amount of spasms my bladder has shrunk significantly. She continued on with a shame train because I refused pharmaceuticals after explaining they didn’t work and made me feel funny. She placed fear deep within my soul threatening that I would need a permanent catheter in my stomach with a bag or bladder augmentation (surgery where they take a piece of your bowel to make you bladder bigger) before I knew it. (see complete Blog entry)
About the Author
JESI STRACHAM is a trauma survivor on a mission to help individuals see the opportunity in their obstacles. She is the founder of Wheel With Me Foundation, the owner of Wheel With Me Consulting, and a fitness and growth coach. Through her struggles, she works for teaching individuals the power of our mindset. Jesi is an honest, authentic, America-loving athlete. Over the past several years, she has generated a significant following among both the spinal cord injury and able-bodied community. Her goal is simple: show the world there is an opportunity in their obstacles, restoring hope during life’s difficult moments. She helps people achieve their dreams through the importance of goal setting, taking control of what we have control over, and showing YOU what’s possible with consistent hard-work.Using Ultrasound for the Evaluation of Incontinence
Written by: Dr. Robert L. Bard
Prolapse of the pelvic floor contents (the uterus, bladder or the anus) is also associated with incontinence. 3-D pelvic floor ultrasound is performed in two ways:1) transvaginal probe which goes inside the vagina
2) transperineal scan which is a more common way for evaluating stress urinary incontinence since the trans perineal probe is applied at the outside of the pelvic floor in the area between the vagina and the anus which is called the perineum.
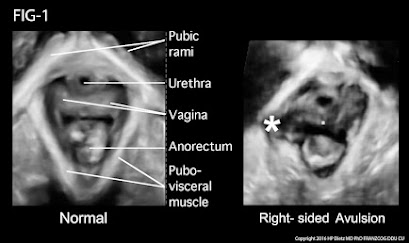
MRI has been used for years to image the prolapse of the pelvic organs but is being replaced by the 4D real time transperineal sonogram as it is quicker and instantaneously shows the tear in the muscular ring (levator sling) that is associated with the trauma of birth. This exam is done in the privacy of an office instead of an MRI center or hospital setting and may be completed in a few minutes by the physician or specially trained technician. The muscle bundle that supports the bladder is white on the sonogram while the tear is black and readily distinguished. During the examination the patient participates actively by bearing down or straining (Valsalva maneuver) to provide an exact measurement of the degree of the descent of the uterus, urethra, bladder or rectum.
Stress urinary incontinence (SUI) is distinct from overactive bladder (OAB) while both may be problematic in older patients with weaker muscle tone. The KEGEL maneuver is a common therapeutic approach to improve muscle strength and diminish the loss of urine when coughing, sneezing or laughing. While the technique is simple, the learning curve is often difficult for women who are accustomed to bearing down rather than “sucking up” the anus or vagina. While 4D ultrasound is optimal for diagnosing the cause, it is sophisticated equipment and requires advanced medical skills. It can go beyond diagnosis and aid in treatment: the demonstration of the bladder change in the proper Kegel contraction is visible to the patients as a dynamic training guide by the physical therapist.
The bladder descends during the Valsava while the bladder and urethra move upward in the correct maneuver. This equipment is portable so it may be brought to the patient rather than a clinic visit or a treatment facility. The technology is also wireless and point of care (POC) images may be transmitted to a reading site for interpretation as is done in ambulances where the EKG is read remotely by the Emergency Department physician while the patient is in route.
FIG-1: Postpartum delivery and difficult childbirth are a major cause of pelvic floor trauma, muscle tears and of course, urinary and fecal incontinence. The ovoid white muscular ring in this case on the right shows a star, which indicates that the white muscular lining, which is smooth on the right hand side of the picture is bulging and actually torn and disappeared by a black area, indicating the exact location at the extent of the tear. This is important preoperatively for reconstructive pelvic floor surgery. While the 3d probe takes 15 seconds to scan the entire pelvic floor surface, it takes training and of course the specialized ultrasound technology, which shows the location and the depth of the disease. More importantly, the patient dynamically assists that is active patient participation to bear down or Valsalva or hold the urine for a varied period of time is important for measuring the descent of the bladder and the uterus in the pelvic floor. Thank you very much for your attention.For the reasons of accurate diagnosis and ease of use, pelvic floor ultrasound is widely used in Europe and becoming popular in the US. The technology is safe and a “black and white” visual aid for learning the Kegel maneuver. Additionally, during the diagnostic evaluation, the physician will look for other etiology of the voiding dysfunction such as bladder stone, bladder cancer and cystitis as well as inflammatory urethritis which is seen with treatments such as transvaginal tape (TVT) or surgical devices that are implanted. Complications of endometriosis and cervical, ovarian or uterine tumors may be detected and definitive treatment may be timely instituted.
Reference:
Dietz, H.P., Pelvic Floor Ultrasound Ultrasound, Atlas and Textbook , 2016 Obstetrics and Gynaeoclogy- Springwood NSW Australia